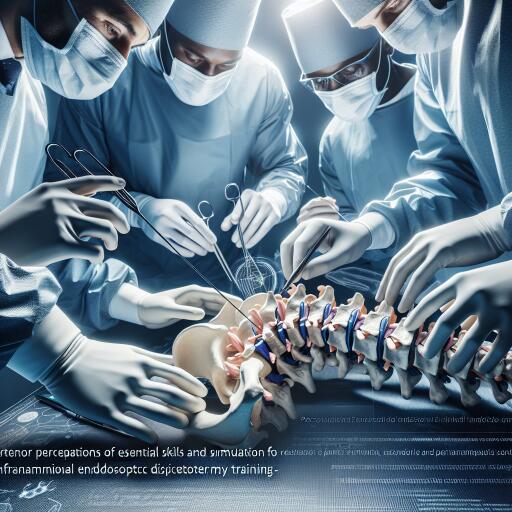
Surgeon perceptions of essential skills and simulation for percutaneous transforaminal endoscopic discectomy training – Scientific Reports
A nationwide snapshot of surgical training in China highlights what spine specialists consider essential for mastering percutaneous transforaminal endoscopic discectomy (PTED) and how simulated environments—especially high-fidelity physical models and virtual reality—are stepping in where traditional cadaver labs are hard to access.
How the snapshot was gathered
An expert-designed, 38-item survey targeting surgeons with PTED experience was circulated through five dedicated spine surgery social groups and at two major orthopaedic meetings. The outreach drew 154 valid responses spanning 22 of the country’s 34 provincial-level regions, representing 64.7% geographic coverage. The result is a broad view of what practitioners believe it takes to perform PTED safely and how they are training the next cohort of endoscopic spine surgeons.
Skills surgeons value most
Respondents placed the greatest emphasis on cognitive competencies—those mental processes that shape safe and efficient decision-making in minimally invasive spine work. These include:
- Spatial reasoning for navigating constrained endoscopic corridors
- Strategic planning of access routes and instrument trajectories
- Real-time interpretation of visual and imaging cues under limited visibility
- Judgment for adapting to variable anatomy and intraoperative surprises
Alongside those cognitive skills, the message was unmistakable: a strong grasp of regional anatomy is non-negotiable for novices aiming to reach proficiency. In PTED, where millimeters matter, anatomical knowledge underpins every move.
Training tools: from cadavers to simulators
Cadaveric practice remains the training modality surgeons prefer, owing to its anatomical realism and tactile nuance. However, younger practitioners reported reduced access to cadaver labs, citing availability and logistical barriers. In that gap, respondents identified two leading alternatives:
- High-fidelity physical models that simulate the lumbar corridor, foraminal relationships, and tool-tissue interactions
- Virtual reality simulators that reproduce endoscopic views, perspective shifts, and procedural choreography without the constraints of lab time
Taken together, these platforms offer scalable, repeatable practice and can be deployed closer to where trainees work—critical advantages for building confidence before operating on patients.
How much simulated practice is typical?
Across respondents, the reported average time in simulated environments reached 22.8 ± 43.6 hours. The broad spread hints at uneven access and differing training cultures—some surgeons log only a handful of hours, while others accumulate dozens. Despite the variability, the trend points toward growing adoption of simulation as a complement to live mentorship and cadaveric experience.
Why this matters for VR and sim-focused developers
For teams building surgical training platforms, the signal is clear: cognitive skill-building should sit at the heart of PTED simulations. That means prioritizing:
- Authentic anatomic fidelity and landmarks for robust spatial orientation
- Convincing endoscopic optics and depth cues to train visual interpretation
- Scenario variability—different disc morphologies, foraminal dimensions, and patient anatomies—to challenge decision-making
- Objective performance analytics that track economy of motion, path planning, and procedural sequence
- Optional haptic feedback or hybrid physical models to approximate tool resistance and contact
Just as importantly, accessibility matters. Portable VR and modular benchtop models can extend high-quality practice to hospitals without cadaver facilities, helping standardize baseline competence across regions.
Key takeaways for PTED education
- Cognition leads: surgeons rate mental frameworks—planning, orientation, and judgment—as the most critical competencies for PTED.
- Anatomy is the foundation: novices progress faster when they train against detailed anatomy, whether on cadavers, high-fidelity models, or well-crafted VR.
- Cadavers are still the gold standard, but access is uneven—especially for younger surgeons.
- High-fidelity physical models and VR simulators are the most favored alternatives, offering repeatability and reach.
- Average simulated practice time reported was 22.8 ± 43.6 hours, underscoring both adoption and variability.
The bottom line
As PTED continues to spread, training needs are evolving. Surgeons prioritize cognitive mastery built on rigorous anatomical understanding. While cadaveric practice remains unparalleled, high-fidelity physical models and VR simulation are emerging as practical, scalable pathways to proficiency—especially for trainees who lack consistent lab access. For the VR and simulation ecosystem, this is a mandate to focus on cognitive load, realism, and measurable skill transfer—bringing surgical education closer to the flexibility, feedback, and immersion that advanced game technology already delivers.