Idaho regulators ordered three insurers to stop limiting Medicare Advantage sales
Idaho’s Department of Insurance has ordered three health insurers to immediately reverse practices that allegedly restricted access to Medicare Advantage (MA) plans during open enrollment, accusing them of intentionally suppressing sales to manage enrollment risk.
Cease-and-desist orders were issued to:
- PacificSource Community Health Plans
- UnitedHealthcare of the Rockies
- Care Improvement Plus South-Central Insurance Co. (a UnitedHealthcare affiliate)
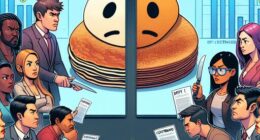
Regulators said they opened an investigation in September after receiving reports that carriers were limiting how consumers and agents could enroll—by restricting online applications and failing to provide sufficient paper forms. Dozens of Idaho agents also told the department the companies planned to stop paying commissions on new MA policies, even though those commissions are built into state-approved rates.
According to the department, company representatives admitted the move wasn’t about cutting costs but about avoiding higher enrollment. Regulators also said they received direct reports from agents that some insurers told them not to market or sell any Medicare Advantage products at all.
By October, department officials allege that UnitedHealthcare executives acknowledged they were discouraging new enrollment “by any means possible.” PacificSource, regulators said, pushed further—pressuring agents to sign new zero-commission contracts by November 1 or risk losing the ability to sell any PacificSource products.
Two subsequent producer bulletins reportedly reinforced a paper-only enrollment push and said commissions were being cut in parts of Idaho due to “market disruptions.” With Medicare open enrollment closing December 7, regulators said swift action was necessary to protect consumers and the agent distribution channel.
What the orders require
Under the cease-and-desist directives, the insurers must:
- Stop any practice that hides, restricts, or delays access to Medicare Advantage applications, online or on paper.
- Restore commissions for new MA enrollments and stop efforts that disincentivize agents from selling MA plans.
PacificSource received an additional order to stop altering agent contracts in ways regulators said were designed to “manipulate the market.”
Company response
UnitedHealthcare said the commission changes only apply to new enrollments and do not affect existing members. In a statement, the company said:
This change is intended to help preserve the benefits that matter most to current members, while supporting the long-term sustainability of these plans in a landscape of increasing regulatory and market pressure.
Why it matters
The stakes are high during Medicare’s annual enrollment window, when seniors evaluate coverage options and pricing for the year ahead. Restricting application channels or cutting agent pay during this period could materially limit consumer choice and access—particularly for people who rely on agents to navigate plan differences, networks, and out-of-pocket costs.
For technology and distribution, the case highlights the critical role of digital access in public program enrollment. Regulators flagged both online application restrictions and shortages of paper forms, underscoring that in today’s hybrid model, throttling either channel can effectively halt sales. With agent commissions embedded in rate filings, unilateral changes can distort the marketplace and undercut the infrastructure that helps consumers compare plans.
The bottom line
Idaho’s move is a clear signal to carriers: curbing access or altering agent incentives to manage enrollment won’t fly—especially during open enrollment with consumer options on the line. The orders require immediate course correction and restore a level playing field for agents and applicants as the December 7 deadline approaches.